For millions of people, milk triggers nothing but abdominal pains, diarrhoea and physical discomfort. This is because they suffer from lactose intolerance, meaning that they lack or are deficient in the enzyme that allows lactose to be broken down in their bodies. The extent to which lactose intolerance affects someone’s quality of life varies from person to person – some people have to completely avoid milk, ice cream and cheese; some experience little discomfort after eating these dairy products.
Around 10,000 years ago, practically everyone suffered from lactose intolerance: even the first farmers who bred cows in Europe could not tolerate lactose. It was only when cattle breeding became more common and milk production increased that people became accustomed to lactose, especially the inhabitants of northern Europe. More lactase developed in their intestines – the enzyme without which the body cannot digest lactose.[18]
Did you know that lactose intolerance is the most common intolerance in the world? Discover more about lactose intolerance symptoms, causes and whether it is possible to treat lactose intolerance. Read on to additionally find out about how other health conditions are believed to be connected with lactose intolerance – including ongoing studies.
What is lactose?
Lactose – that is, milk sugar – is a disaccharide which consists of glucose (grape sugar) and galactose. Lactose can be found mainly in milk of mammals and derived milk products such as cheese, curd and cream cheese. The lactose content varies according to the production process. Hard cheeses contain less lactose than cream cheese, as lactic acid bacteria break down lactose.[1]
As a young child, lactose is the only source of carbohydrate that we take in through our mother’s milk. It helps us develop healthy gut flora and promotes calcium absorption for bone formation.[19, 20]
Did you know that breast milk contains more lactose than cow’s milk?[21]
What is lactose intolerance?
Lactose intolerance is a food intolerance that inhibits sufferers from being able to absorb lactose. In order to be adequately digested in our gut, lactose must be broken down into its chemical components. This is done by means of lactase – an enzyme. People with lactose intolerance either completely or partially lack this enzyme in their bodies. As a result, lactose cannot be broken down and utilised, causing gastroenteric symptoms.[1]
When lactose is not broken down into glucose and galactose and is transported undigested into the large intestine, the gut bacteria utilise this form of lactose and produce hydrogen, methane and short-chain fatty acids. Carbon dioxide causes lactose intolerance symptoms such as flatulence and bad breath. The fatty acids take water from the intestine and dilute the stool, resulting in diarrhoea. Combined, these gases cause bowel sounds, tiredness and heartburn.[3]
What are typical symptoms of lactose intolerance?

Symptoms of lactose intolerance are relatively clear. After drinking a glass of milk, the following gastrointestinal symptoms will occur:[1]
- flatulence
- diarrhoea, constipation
- stomach cramps, stomach pains
Headaches and migraines with nausea and vomiting can be further generic lactose intolerance symptoms.[1]
When do symptoms of lactose intolerance occur?
When exactly symptoms occur depends on the activity of the lactase. Perhaps your stomach makes itself felt by loud sounds just 30 minutes or a few hours after you eat foods containing lactose.[3]
Did you know that you don’t need to be lactose intolerant to experience diarrhoea? Large quantities of foods containing lactose can have laxative effects – even in people with normal lactase activity.
Lactose intolerance versus dairy allergy: the difference
Again and again, a lactose intolerance and dairy allergy are lumped together as one condition, as milk triggers of the symptoms for both of them. But other than this trigger, these two conditions don’t have much in common: where an allergy involves the immune system, an intolerance has little to do with the immune system.
Here are some of the main differences between a lactose intolerance and milk allergy.[22]
|
|
Lactose intolerance |
Milk allergy |
|
Type of condition |
Intolerance |
Food allergy |
|
Trigger |
Lactose (sugar in milk) |
Milk proteins: casein, whey |
|
Cause |
Enzyme deficiency (lactase) |
Immune response (production of antibodies) |
|
Parts of the body most affected |
Gastrointestinal tract |
Gastrointestinal tract, skin, respiration |
To find out more about the difference between a food allergy and intolerance, read our dedicated Health Portal article.
Lactose intolerance causes
What are causes of lactose intolerance?
The causes of lactose intolerance depend on the type of lactose intolerance. It is clear that too low production of lactase in the small intestine causes unpleasant gastrointestinal symptoms. The intensity of the symptoms is very individual and depends on the level of the intolerance. In other words: how much lactase is still produced and how much lactose is consumed.
Does lactose intolerance get worse with age?
Can you develop lactose intolerance? One thing is certain: The body’s own production of lactase in the small intestine drops in infants as of the start of weaning and continues to decline with age. One reason is that mothers supply their babies with milk during breastfeeding. The human body produces enough lactase during this time. Once babies no longer feed on this breast milk, lactase production starts to decrease. This physiological lactase deficiency, also known as hypolactasia, is widespread throughout the world.[2] In how far lactase production drops after being weaned off breast milk varies from person to person.[2]
If a child cannot tolerate milk, it might have a milk allergy. This occurs especially in early childhood.
Can lactose intolerance run in families?
Primary lactase deficiency is a genetic lactase deficiency whereby drastically less lactase is produced as a result of genetics. This type of deficiency is very rare. If this disease is not treated at an early stage, it can cause growth and developmental disorders in children.[2]
There is furthermore a theory that lactose intolerance can be genetically determined. Asians and South Africans especially suffer from lactose intolerance; Europeans and North Africans, however, can enjoy their glass of milk in the morning. But why is this?
Experts have discovered a correlation between lactose intolerance and the introduction of farming by certain nomadic populations. As mankind at that time lived together with cows and drank a lot of milk, they started to produce lactase. Milk served as a staple food, which is certain people tolerate milk much better than other people.[5]
Which other health conditions can trigger lactose intolerance?
A secondary lactase deficiency is caused by an underlying illness – that is, where the mucous membrane is damaged by Coeliac disease, Crohn’s disease or ulcerative colitis, for example. This type of deficiency can begin at any age. When the symptoms of the underlying disease can be alleviated, the symptoms of lactose intolerance mostly decrease as well.[2]
How common is lactose intolerance?
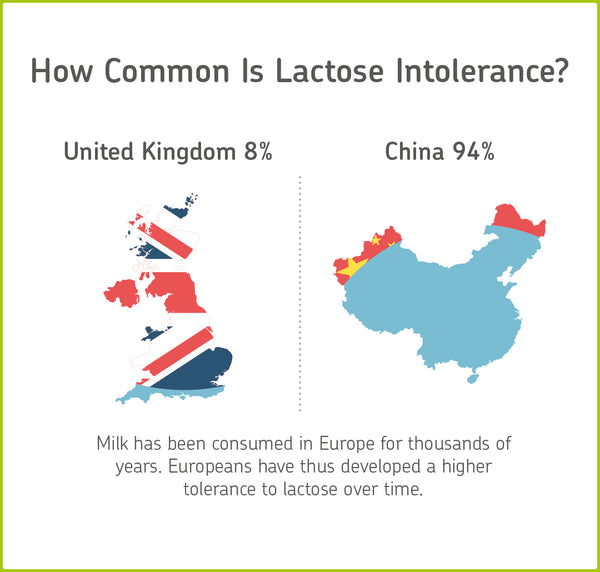
Worldwide, 75 per cent of adults are affected by lactose intolerance. In the United Kingdom, eight per cent of people are unable to digest lactose contained in foods. Speaking generally, in Northern Europe, fewer people suffer from lactose intolerance than in southern Europe.[2]
In Sweden, only five per cent of the population are affected, whereas in southern Italy, 68 per cent of the population suffer from lactose intolerance. Asians hardly or cannot tolerate milk. In Japan, up to 98 per cent of the population suffers from this intolerance.[2]
How lactose intolerance is diagnosed
Even if symptoms of lactose intolerance are very clear and occur directly after consumption of milk and dairy products, a lactose test provides clarity and, above all, security. Leaving out foods without any evidence of an intolerance should be a last resort – otherwise, this can quickly lead to nutrient deficiencies. Lactose intolerance tests are pain-free and don’t require taking blood samples, as they require breath samples instead.
How do I get tested for lactose intolerance?
Diagnosing lactose intolerance is literally only a breath away. To confirm this intolerance, all you need to do is perform a hydrogen breath test (H2 breath test). The breath test measures hydrogen and methane levels in your breath. The H2 breath test is the gold standard when it comes to diagnosing lactose intolerance. After drinking a liquid solution containing lactose, breath samples are taken after several intervals. The concentrations of hydrogen and methane are measured in these breath samples, as these are produced if you are intolerant to lactose.[12]
As approx. 35 per cent of people do not exhale enough hydrogen, methane concentration is also measured in the air exhaled. Methane is another gas that is produced in greater quantities if there is an intolerance.
A lactose intolerance test generally takes – depending on the number of samples required – up to three hours. During this period, you need to fast. It is best to perform the test at home, as you would otherwise have to stay at the doctor’s for up to three hours. If you are intolerant to lactose, unpleasant lactose intolerance symptoms may also occur.
Testing for lactose intolerance test can, however, also be carried out by your family doctor or allergist. These doctors also use breath tests.
What are the parameters investigated with a lactose intolerance test?
When analysing samples taken with a lactose intolerance test, the concentration of hydrogen and methane over the fasting period are calculated. The samples are taken every 30 minutes after the liquid solution containing lactose has been ingested. If the hydrogen analysis reveals a difference of 20 ppm (parts per million) and/or for methane of 12 ppm, it is very likely that you have a lactose intolerance. If the methane concentration is smaller, hydrogen values are the decisive parameter.
|
Example of hydrogen breath test analysis |
|
|
Hydrogen analysis |
|
|
difference after 30 minutes |
8 ppm |
|
difference after 60 minutes |
22 ppm |
|
difference after 120 minutes |
7 ppm |
|
difference after 180 minutes |
0 ppm |
|
Is there a difference of at least 20 ppm? Yes |
|
|
Methane analysis |
|
|
difference after 30 minutes |
3 ppm |
|
difference after 60 minutes |
10 ppm |
|
difference after 120 minutes |
12 ppm |
|
difference after 180 minutes |
14 ppm |
|
Is there a difference of at least 12 ppm? Yes |
|
Should diabetics avoid lactose?
At a first glance, lactose intolerance and diabetes don’t seem to have much in common. In practice, however, diabetics often mention symptoms which suggest lactose intolerance – such as flatulence, constipation or diarrhoea.
In 2016 a large-scale study revealed a correlation between type 2 diabetes and lactose intolerance. The study compared the presence of lactose intolerance in diabetes patients with healthy participants and resulted in an interesting finding. Considerably more diabetics are affected by lactose intolerance. Why lactose intolerance occurs more often and whether there is a correlation between lactose intolerance and insulin has not yet been clarified.[13]
In another study, scientists showed that refraining from eating dairy products increases the risk of type 2 diabetes. The reason behind this is a calcium deficiency. Study participants who consciously avoided milk products were at a higher risk of developing type 2 diabetes. They didn’t eat dairy products, as they suspected they were lactose intolerant. However, this assumption was not based on a doctor’s diagnosis or a lactose intolerance test.[14]
Diabetics have to take into consideration the consumption of foods containing lactose to calculate their insulin dose. Lactose, a sugar found in milk, is normally broken down into its components glucose and galactose. Glucose causes a rise in blood sugar levels. Diabetics have to counter this rise with insulin. Milk products which do not contain added sugar (plain yogurt), ensure that blood sugar levels rise more slowly. [15]
Lactose intolerance does not automatically lead to type 2 diabetes. But if you consciously avoid dairy products due to a mere suspicion that you are lactose intolerant, this can cause a calcium deficiency. Calcium deficiency can, in return, increase the risk of diabetes. Therefore, a suspected lactose intolerance should certainly be clarified.
If you feel discomfort after eating certain foods, do not avoid them for a long period of time. Consult a doctor or perform an at-home intolerance test to determine whether you have an allergy or intolerance. Self-diagnosis can lead to nutrient deficiency!
Can lactose intolerance affect your skin?

Milk products are suspected to be associated with the development of acne and pimples. Whether there really is a correlation is not clear considering recent studies. The hormones and proteins found in milk are suspected triggers for skin impurities. Thus, there is no direct correlation between lactose intolerance and skin impurities. Blemishes caused by milk are more often caused by milk allergy. [16]
Does lactose cause depression?
A survey has in fact revealed a correlation between lactose intolerance and depression. Female survey participants filled in a questionnaire used for diagnosing depression. The evaluation showed that women with lactose intolerance had a stronger tendency towards depressive symptoms than healthy women due to the deficiency of a certain amino acid (L-tryptophan). The main function of this amino acid is to produce happiness, so to speak, as the body transforms it into serotonin – also known as the happiness hormone. [17]
The fact that lactose intolerance could be linked with depression is a general statement, however, and recommendations for action cannot be given.
Can lactose cause shortness of breath?
Symptoms of lactose intolerance mainly involve the gastrointestinal tract. Lactose intolerance symptoms therefore do not include asthma or difficulties breathing. If you feel respiratory problems after consumption, you should do a test for milk allergy.[12]
Lactose intolerance treatment

If you are diagnosed with lactose intolerance, you first have to avoid foods containing lactose. Depending on the intensity of your symptoms, foods containing lactose can be added to your diet in small amounts. Please read on to learn how to integrate foods containing lactose into your diet without triggering symptoms.
How do you treat lactose intolerance?
The correct lactose intolerance treatment method depends on the severity of the intolerance. This will determine to which degree someone has to reduce or even avoid their lactose consumption. If the intolerance is caused by an underlying disease such as Coeliac disease, lactose must be avoided. Otherwise, you can follow the subsequent steps to treat lactose intolerance.[3]
Can you use the elimination diet for lactose intolerance?
After being diagnosed with lactose intolerance, you may need to change your everyday diet. This means that foods containing lactose should be eliminated from your diet. This elimination diet consists of three phases, which slowly help you figure out how much lactose you can tolerate.
Phase 1: abstaining from consuming lactose
For a maximum period of two weeks, you follow a lactose-free diet. You additionally avoid sugar alcohols (sorbitol, xylitol, maltitol, mannitol and isomalt), which also trigger lactose intolerance symptoms. The aim is to eliminate symptoms as far as possible.
Phase 2: test phase
During this period, foods containing lactose (incl. milk and dairy products) are gradually reintroduced into the diet. This way, your individual tolerance threshold can be determined. Start with very small amounts of those foods and gradually increase them. Stop this phase of testing when the first symptoms appear. The aim here is to find out your tolerance threshold. This way, you know exactly how much milk and dairy products you tolerate, so you don’t have to completely avoid foods containing lactose.
Phase 3: permanent diet
The third and final phase is considered important for determining your permanent diet. It is best to check which foods have a high lactose content. People who produce little lactase must avoid even small quantities of lactose and follow a strictly lactose-free diet. Most people affected by lactose intolerance do not have to follow such strict diet, as their lactase production normally is not that low. With a moderate lactose intolerance, up to ten grammes of lactose per day can be tolerated.
Practical experience has shown that consuming small amounts of lactose (less than three grammes) seldom causes reactions. Foods with low-lactose content can mostly be consumed without problems. Lactose intolerance symptoms often occur when more than ten grammes of lactose are consumed.
|
Selected foods |
Content of milk sugar in g/100g |
|
Cow’s milk |
4.8 |
|
Curd (low-fat) |
4.1 |
|
Plain yogurt |
4 |
|
Yogurt (with skimmed milk powder) |
5.3 |
|
Processed cheese |
8.9 |
|
Cream cheese |
3.4 |
Are there lactose intolerance pills?
When you switch to a lactose-free diet or a diet low in lactose, it is possible to consume lactase enzyme tablets or capsules. These are often known as lactose intolerance pills. You have to take them before you consume foods containing lactose. Whether they are effective or not varies from person to person.
First, you have to determine the right dosage you need to avoid symptoms. Lactose intolerance pills should, however, only be taken in exceptional cases, as the constant use of these tablets decreases the remaining lactase activity in your body. As a result, foods containing lactose are less tolerated than before the test phase. People who are lactose intolerant should instead change their diet so that their colon can recover.
What foods should you avoid if you are lactose intolerant?

Lactose is above all found in milk and dairy products such as curd, cheese, cream cheese, mozzarella and yogurt. Cow’s milk, sheep’s milk and goat’s milk also contain lactose and must be avoided as well.
Foods with a high lactose content are listed below. If you suffer from lactose intolerance, these foods can be eaten in smaller amounts. You have to individually test how severe your intolerance is. Start with very small amounts and gradually increase them. When gastrointestinal symptoms reoccur as of a certain amount, you should stop consuming any more lactose. This way, you can find out the limit of your individual tolerance. A food diary can be helpful.
|
Food group |
Foods containing lactose |
|
milk/dairy products |
Milk, cheese, dry milk, mixed drinks, hot chocolate, desserts, condensed milk, cream, sour cream, kefir, yogurt, curdled milk, whey, curd, cottage cheese, processed cheese, cheese |
|
Bread/baked goods |
Milk and/or milk powder can be found in: bread and cake baking mixtures, brioche, waffles, cakes, cookies, crackers |
|
Ready meals |
Pizza, frozen prepared dishes |
|
Confectionery |
Ice cream, chocolate, toffees, chocolate bars, nougat, hazelnut spread |
|
Meat/cold meats |
Sausages, liver sausage, fat-reduced cold meats, sausage meat |
|
Instant products |
Instant soups, instant sauces, mashed potato |
|
Ready-made sauces |
Gourmet and barbecue sauces, salad dressings |
|
Other products |
Muesli, granola, margarine products, spreads |
How do you get calcium if you are lactose intolerant?
Everyone knows that milk contributes to maintaining healthy and strong bones. This is because milk contains calcium which is vital for the construction of bones and teeth, for muscle contraction and blood clotting. Calcium deficiency disrupts the micro-architecture of bone tissue by causing osteoporosis, caries and heart problems.[11] If you are lactose intolerant, calcium supplements should be considered if you receive no other calcium source through your diet.Did you know why lactose-free milk tastes sweeter? Lactose-free milk contains the enzyme lactase. Thus, the lactose of the milk is already split up into its components.
Hitting the supermarkets with lactose intolerance
Foods ideal for lactose intolerance
Apart from the numerous lactose-free food alternatives, there are lots of foods that are naturally lactose-free. Even if the market for lactose-free products is booming, you do not necessarily have to replace all dairy products by lactose-free alternatives. Some cheeses and butter are low in lactose. The following cheeses can be enjoyed without you worried about symptoms:[8]
- Emmental cheese
- Cheddar cheese
- Swiss cheese
- Parmesan cheese
The softer the cheese, the more lactose it contains. Mozzarella, for example, contains three grammes of lactose per 100 grammes. Gouda cheese with 45 per cent fat, however, contains less than 0.1 grammes of lactose and is classed as lactose-free.[9]
Did you know that all products with less than 0.1 grammes lactose per 100 grammes may be labelled lactose-free!
Low-fat curd is considered to be a top post-workout snack. It is an ideal snack not only for bodybuilding, but also for weight loss! But beware: it contains approximately three grammes of lactose.[9] For unpacked foods, for example, when you’re eating out, we recommend asking a member of staff in the establishment.
You must also be careful with medicines as these could also contain lactose. Many manufacturers meanwhile declare on their own whether their products are lactose-free - sometimes in the form of a seal, sometimes clearly visible in the form of a word.[11]
Did you know that 80 per cent of people buying lactose-free products do not suffer from an intolerance. There is a myth that lactose-free foods are healthier. Lactose-free foods are no “wonder weapon” for a healthier lifestyle. Whether or not foods contain lactose does not contribute to a healthier life without intolerances![10]
Lactose intolerance – at a glance
What is lactose intolerance?
Lactose intolerance stops certain people from being able to absorb lactose. In order to be adequately digested in our gut, lactose must be broken down into its chemical components. For this process, we need enough of the lactase enzyme. People with lactose intolerance either completely or partially lack this enzyme in their bodies. As a result, lactose cannot be broken down and utilised, causing various uncomfortable symptoms.[1]
What are symptoms of lactose intolerance?
Symptoms of lactose intolerance are flatulence, stomach cramps, stomach pains, diarrhoea and constipation.
Are there lactose intolerance treatment methods?
Lactose intolerance treatment can involve the elimination diet – that is, eliminating and then reintroducing lactose into the diet – lactose intolerance pills, or completely avoiding lactose altogether. If you cannot tolerate any amount of lactose, you should make sure that you still receive sufficient nutrients, such as calcium.
Sources
- Laktoseintoleranz: Nicht alle Milchprodukte unverträglich, https://www.bzfe.de/inhalt/laktoseintoleranz-29171.html
- Laktose-Intoleranz - Milchzucker-Unverträglichkeit - Laktasemangel - BGV Info Gesundheit e.V., http://www.bgv-laktose.de/milchzucker.html
- Kasper, H.: Ernährungsmedizin und Diätetik. Urban & Fischer Verlag/Elsevier GmbH (2014)
- Lactose Intolerance vs. Dairy Allergy, https://www.webmd.com/digestive-disorders/lactose-intolerance-or-dairy-allergy
- Absence of the lactase-persistence-associated allele in early Neolithic Europeans | PNAS, http://www.pnas.org/content/104/10/3736
- Rationalisierungsschema, http://daem.de/index.php/veroeffentlichungen/rationalisierungsschema
- Treatment, https://www.nhs.uk/conditions/lactose-intolerance/treatment/
- Hartkäse und Weichkäse - Lebensmittel-Warenkunde, https://lebensmittel-warenkunde.de/lebensmittel/milch-milchprodukte/kaese/hartkaese-weichkaese.html
- Die Zusammensetzung der Lebensmittel, Nährwert-Tabellen. (2016)
- “... frei von Laktose” - BZfE, https://www.bzfe.de/inhalt/pressemeldung-6233.html
- EU03_2010_markt_produkte.qxd.pdf, https://www.ernaehrungs-umschau.de/fileadmin/Ernaehrungs-Umschau/pdfs/pdf_2010/03_10/EU03_2010_markt_produkte.qxd.pdf
- Laktose-Intoleranz: DAAB, http://www.daab.de/ernaehrung/laktose-intoleranz/
- Rana, S., Morya, R.K., Malik, A., Bhadada, S.K., Sachdeva, N., Sharma, G.: A relationship between vitamin D, parathyroid hormone, calcium levels and lactose intolerance in type 2 diabetic patients and healthy subjects. Clin. Chim. Acta. 462, 174–177 (2016). doi:10.1016/j.cca.2016.09.009
- Gao, D., Ning, N., Wang, C., Wang, Y., Li, Q., Meng, Z., Liu, Y., Li, Q.: Dairy Products Consumption and Risk of Type 2 Diabetes: Systematic Review and Dose-Response Meta-Analysis. PLoS ONE. 8, e73965 (2013). doi:10.1371/journal.pone.0073965
- Frühstück: So schaffen Sie eine gesunde Grundlage, https://www.diabetes-ratgeber.net/Ernaehrung/Fruehstueck-So-schaffen-Sie-eine-gesunde-Grundlage-225707.html
- Melnik, B.C.: Evidence for Acne-Promoting Effects of Milk and Other Insulinotropic Dairy Products. Milk Milk Prod. Hum. Nutr. 67, 131–145 (2011). doi:10.1159/000325580
- Ledochowski, M., Sperner-Unterweger, B., Fuchs, D.: Lactose malabsorption is associated with early signs of mental depression in females: a preliminary report. Dig. Dis. Sci. 43, 2513–2517 (1998)
- Y. Deng, B. Misselwitz, N. Dai, und M. Fox, „Lactose Intolerance in Adults: Biological Mechanism and Dietary Management“, Nutrients, Bd. 7, Nr. 9, S. 8020–8035, Sep. 2015, doi: 10.3390/nu7095380.
- I. Elmadfa, Ernährungslehre, 3. Aufl. Verlag Eugen Ulmer Stuttgart, 2015.
- Y. Vandenplas, „Lactose intolerance“, Asia Pac J Clin Nutr, Bd. 24 Suppl 1, S. S9-13, 2015, doi: 10.6133/apjcn.2015.24.s1.02.
- N. Silanikove, G. Leitner, und U. Merin, „The Interrelationships between Lactose Intolerance and the Modern Dairy Industry: Global Perspectives in Evolutional and Historical Backgrounds“, Nutrients, Bd. 7, Nr. 9, S. 7312–7331, Aug. 2015, doi: 10.3390/nu7095340.
- J. Walsh, R. Meyer, N. Shah, J. Quekett, und A. T. Fox, „Differentiating milk allergy (IgE and non-IgE mediated) from lactose intolerance: understanding the underlying mechanisms and presentations“, Br J Gen Pract, Bd. 66, Nr. 649, S. e609–e611, Aug. 2016, doi: 10.3399/bjgp16X686521.